- Fellow Highlights
COVID-19: Paul & Daisy Soros Fellows in Public Health and Health Care
The following Paul & Daisy Soros Fellows are working to support the delivery and implementation of health care and public health measures at the national, state, local, and hospital level. All of them are immigrants and children of immigrants. We’ll continue to update this list.
Ashish Agrawal (2009 Fellow), is an assistant clinical professor of anesthesiology at UCSF, and is based at Zuckerberg San Francisco General Hospital. In addition to direct clinical care, Ashish, who is the child of immigrants from India, has four main administrative roles: First, he’s the medical director for respiratory care services, and he has been supervising an incredible multidisciplinary team of respiratory therapists to ensure that they have adequate ventilators, viral filters, and other supplies as well as working on increasing their respiratory therapist staffing throughout the hospital to meet the increased needs.
Second, Ashish directs the residents and fellows who rotate through the hospital’s ICU, and they have put in a lot of effort to ramp up the workforce, adjust clinical schedules to meet the additional demand, and make sure that their trainees have the emotional support and time off to recharge during this difficult time.
Third, Ashish been helping staff at the county and state level as a ventilator content expert, reviewing specifications for new ventilators that have been approved under an FDA emergency authorization to see whether they would meet their clinical need for COVID-19 patients.
And lastly, Ashish has been working with his department and with hospital leadership on an incredible number of rapidly evolving new protocols for taking care of patients as well as to prepare to expand their ICU to new locations, such as the operating rooms, should they run out of physical bed spaces to properly manage their care.


Nadine Burke-Harris (1999 Fellow), the surgeon general of California, has been working tirelessly to support public health efforts in our state and across the country. California rolled out a new campaign on COVID-19, which features a PSA by Nadine. She’s done Q&As with public figures like Kerry Washington and Nadine has been on a Nickelodeon special with Kristin Bell geared towards helping parents talk to their children about the pandemic.
Chiara Galimberti (2011 Fellow), originally from Italy, and currently residing in Chicago, is an acupuncturist, organizer, artist, immigrant, and former teen mother living with a disability. During the COVID pandemic, she has published a free at-home care support document from a traditional Chinese medicine perspective, and is currently working on an accessible acupressure guide for people who do not have access to their medical provider during the quarantine. She is also offering free and donation-based remote care for low-income people in Chicago. Chiara has a master’s in acupuncture and is a licensed and board-certified acupuncturist.


Sumeet Garg (2002 Fellow), the child of immigrants from India, is an associate professor of orthopedics at the University of Colorado where he works at Children’s Hospital Colorado. Sumeet explained that all of his elective surgeries have been cancelled, but he is providing care for spinal deformities and diseases by telehealth, and taking care of orthopedic emergencies in children on-call including surgery when needed. Sumeet is the director of quality for his group, and is leading quality improvement projects for the team members who have had a decline in their clinical roles by cancellation of elective appointments and surgeries. “Being a specialist that’s not directly related to ER, ICU, or pulmonary disease you feel somewhat on the outside while colleagues are handling the very sick patients suffering from this disease,” Sumeet explained. “I do still feel we are playing a role as children continue to be injured, sustain fractures and dislocations, and bone and joint infections and deserve our highest care even in this challenging health care environment.”
Woong Y. Hwang (2019 Fellow) is a sixth year MD/PhD student at Yale School of Medicine. Due to the current COVID-19 pandemic, Woong explained that thousands of patients appointments at Yale New Haven Hospital have been cancelled. In an effort to help lighten the workload from healthcare providers who are at the frontline of this pandemic, Woong joined the Medical Student Task Force (MSTF), which is a student initiative patient outreach program at Yale School of Medicine. As part of the program, student volunteers call patients to check if they have any urgent medical or prescription needs and relay the information to the patients’ providers.
“As a medical trainee, I have not mastered clinical knowledge and skillset to combat this pandemic at the frontlines yet, but we can still meaningfully contribute by providing virtual care to non-COVID19 patients to ease clinician’s workload so that they have more time allocated to treat patients with COVID-19. We are not sidelined,” Woong said. “We are part of much large clinical team in this battle against COVID-19. Medicine is a privilege that comes with great responsibility. This valuable experience gained from this once in a lifetime public health crisis will better prepare next-generation healthcare professionals to combat the next possible pandemic in the future.”
Woong was born and raised in Seoul, South Korea until he was fifteen. Woong’s mother saw an opportunity to work as a nurse in the United States, and despite the language barrier, she received the sponsorship and the permanent residency for his family. Woong’s mother worked as a nurse in both South Korea and the United States for 30 years and recently retired. In response to the call for help in the battle against COVID-19, she jumped back into service and is now working as a registered nurse at the hospital in Washington where the first COVID-19 patient death was reported in the United States. Woong writes, “She is my true inspiration and role model I would like to emulate in my role as a physician in the future.”

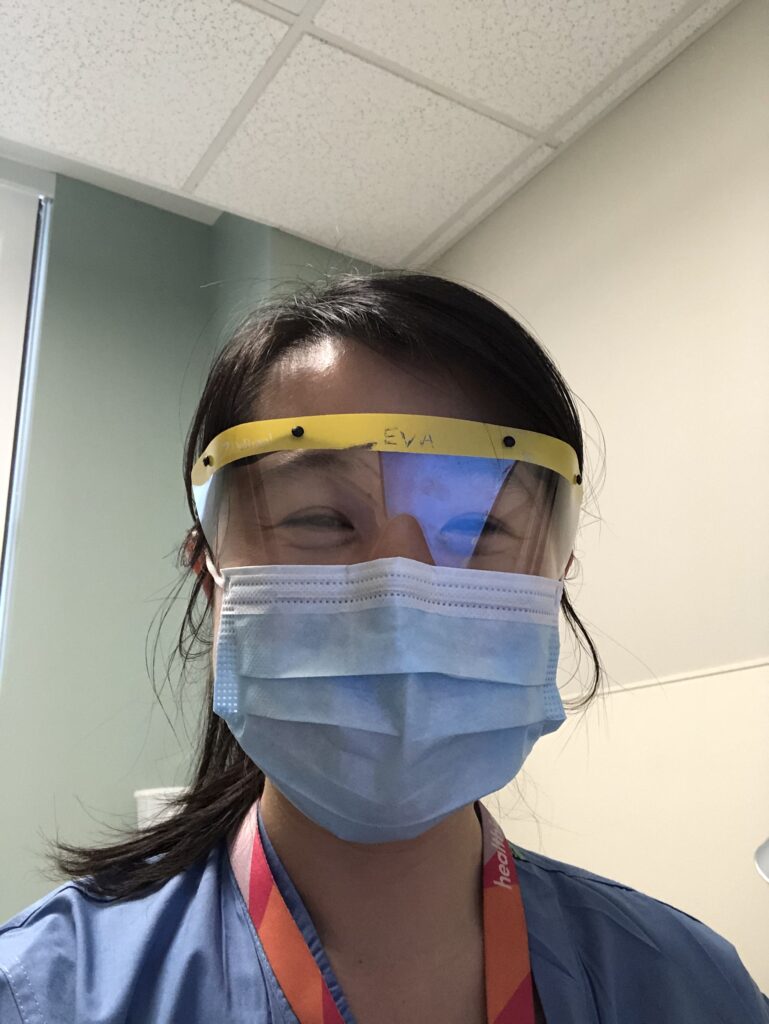
Eva Luo (2012 Fellow) is working administratively at Harvard Medical Faculty Physicians at Beth Israel Deaconess Medical Center, Inc. where her primary role is to provide regular, daily communications to their providers across the entire Beth Israel Lahey network about coronavirus and to help ramp of telehealth services. Eva is working on everything from the technology to the staff workflow operations to billing and tracking of services provided for the use of telehealth by the network, which cares for roughly a quarter of Massachusetts’s population. Eva explained, “Telehealth is a big change for health care, much needed and will be here to stay.”
Eva was born in Florida to parents who had, only a year prior to having Eva, reached the United States in the aftermath of the Chinese Cultural Revolution. She is a graduate of Harvard Medical School and Harvard Business School. “As a medical trainee, I have not mastered clinical knowledge and skillset to combat this pandemic at the frontlines yet, but we can still meaningfully contribute by providing virtual care to non-COVID19 patients to ease clinician’s workload so that they have more time allocated to treat patients with COVID-19. We are not sidelined,” Woong said. “We are part of much large clinical team in this battle against COVID-19. Medicine is a privilege that comes with great responsibility. This valuable experience gained from this once in a lifetime public health crisis will better prepare next-generation healthcare professionals to combat the next possible pandemic in the future.”
Woong was born and raised in Seoul, South Korea until he was fifteen. Woong’s mother saw an opportunity to work as a nurse in the United States, and despite the language barrier, she received the sponsorship and the permanent residency for his family. Woong’s mother worked as a nurse in both South Korea and the United States for 30 years and recently retired. In response to the call for help in the battle against COVID-19, she jumped back into service and is now working as a registered nurse at the hospital in Washington where the first COVID-19 patient death was reported in the United States. Woong writes, “She is my true inspiration and role model I would like to emulate in my role as a physician in the future.”
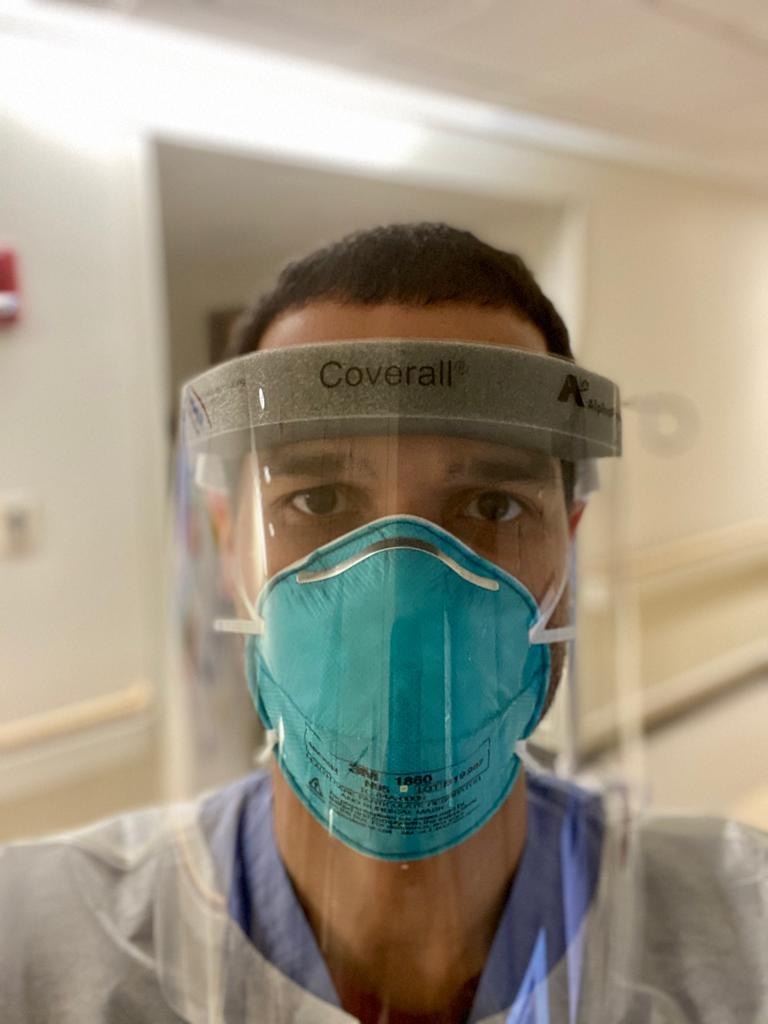
Wilfredo Matias (2013 Fellow), an immigrant from the Dominican Republic, is serving patients and is a fellow in global health at the Massachusetts General Hospital Center for Global Health, where they are working closely with partners in Haiti, the Dominican Republic, Uganda and elsewhere to prepare for the impending pandemic in areas of the world where medical and public health resources are severely limited. “I am concerned by how this pandemic has challenged some of the most developed health systems in the world. When I think of my friends and family in less privileged parts of the world where resources are scarce, such as in Haiti or the Dominican Republic, I worry about the staggering effect that this pandemic could have on places where oxygen, let alone a ventilator, is hard to come by,” Wilfredo said. “As we overcome the pandemic here at home, it is our moral imperative to help our brothers and sisters in rest of the world, who may yet bear the worst burden of this pandemic.”

Vivek Murthy (1998 Fellow), the former United States Surgeon General and an immigrant from England, has been educating the public regularly through widely distributed interviews, articles, and speeches. He has also been speaking directly to health care professionals and recently co-wrote an open letter of gratitude to them. An expert on loneliness, Vivek has focused much of his recent comments on how Americans can maintain strong social connections while social distancing.
Rahul Rajkumar (2004 Fellow), the SVP & chief medical officer at Blue Cross Blue Shield North Carolina, explained that “The pandemic has changed my job in many ways—and has accelerated our work in others.”
Blue Cross Blue Shield North Carolina was one of the first health plans in the country to announce full payment for telehealth for all providers and all specialties at parity with face-to-face visits and to waive cost-sharing for all COVID-19 testing or treatment-related member cost sharing. They have played a major role in helping North Carolina providers secure personal protective equipment—including obtaining machines for the local automated production of N95 masks in North Carolina.


Elsie Gyang Ross (2008 Fellow) is a vascular surgeon and research scientist at Stanford University who kept her research lab running during the pandemic despite being on maternity leave. One of the lab’s current research projects is evaluating the change in vascular surgeries across the nation attributed to COVID-19 by looking at how COVID affected the elective and the urgent and emergent volumes of surgery. “I see this as a public health issue as many people have been foregoing surgery but in the vascular surgery world, diseases due to atherosclerosis don’t get better and can continue to get worse,” Elsie explained. “So our goal is to measure how much things have changed so that we know where we need to focus our efforts to ensure people don’t permanently fall through the cracks.”
Lorenzo Sewanan (2017 Fellow) is volunteering as a research assistant with Yale School of Medicine Professor Albert Ko’s team, which is conducting a study to prospectively screen health care workers including nurses, patient care assistants, respiratory technicians, doctors, and other health care staff that are actively exposed to COVID positive patients in the hospital as part of their work. “Our work allows early detection of SARS-CoV-2 infection of health care workers using viral nucleic acid diagnostics, often before the onset of symptoms, allowing us to make recommendations for quarantine and additional screening of individuals and their associated contacts,” Lorenzo explained. “Furthermore, we are collecting longitudinal symptom data, exposure and personal protective equipment data, and biological data such as antibody levels, blood biomarkers, and viral titers. We hope to produce research allowing us to understand factors influencing infection rate and exposure of health care workers and proper ways to protect them and limit risk, helping to keep our healthcare workforce healthy. For me, it’s been particularly exciting to be immersed in this type of clinical research that feels very relevant in the current pandemic; I’m inspired to pursue more work like this in the future.” The work is conducted by a team that includes two infectious disease fellows, Melissa Campbell and Rupak Dhatta, a group of medical students including Lorenzo, Ryan Handoko, Nida Naushad, and Jordan Valdez, the dedicated support staff at the Yale Center for Clinical Investigation HRU, and other infection control staff at Yale New Haven Hospital and Yale School of Medicine.


Nirav Shah (2005 Fellow), is leading the state-wide effort against COVID-19 in Maine where he is the director of the Maine Center for Disease Control and Prevention. Learn more about his work here. Nirav is the child of immigrants from India.
Featured Fellows
-

Ashish Agrawal
Physician, UCSF Medical Center
Ashish Agrawal is the child of immigrants from India. Fellowship awarded in 2009 to support work towards an MD at University of California, San Francisco School of Medicine
-

Nirav Shah
Principal Deputy Director, Centers for Disease Control
Nirav Shah is the child of immigrants from India. Fellowship awarded in 2005 to support work towards an MD in Medicine at University of Chicago
Keep Exploring
-
 Read more: The Public Voices Fellowship of PD Soros, in partnership with the Oped Project: Year Four
Read more: The Public Voices Fellowship of PD Soros, in partnership with the Oped Project: Year FourThe Public Voices Fellowship of PD Soros, in partnership with the Oped Project: Year Four
-
Read more: NOT ON MY RESUME: Ming Hsu Chen
- Fellow Highlights
- Fellows in Action
NOT ON MY RESUME: Ming Hsu Chen
-
 Read more: Kathy Ku Steps into Leadership as PDSFA Chair
Read more: Kathy Ku Steps into Leadership as PDSFA Chair- Board of Directors
- Fellowship News
Kathy Ku Steps into Leadership as PDSFA Chair
-
 Read more: Q&A with MD/PhD Student Silvia Huerta Lopez
Read more: Q&A with MD/PhD Student Silvia Huerta LopezQ&A with MD/PhD Student Silvia Huerta Lopez
