- Fellow Highlights
Shantanu Nundy’s Blueprint for Rethinking Healthcare in a Post-Pandemic World
By 2020 Paul & Daisy Soros Fellow Sherman Leung
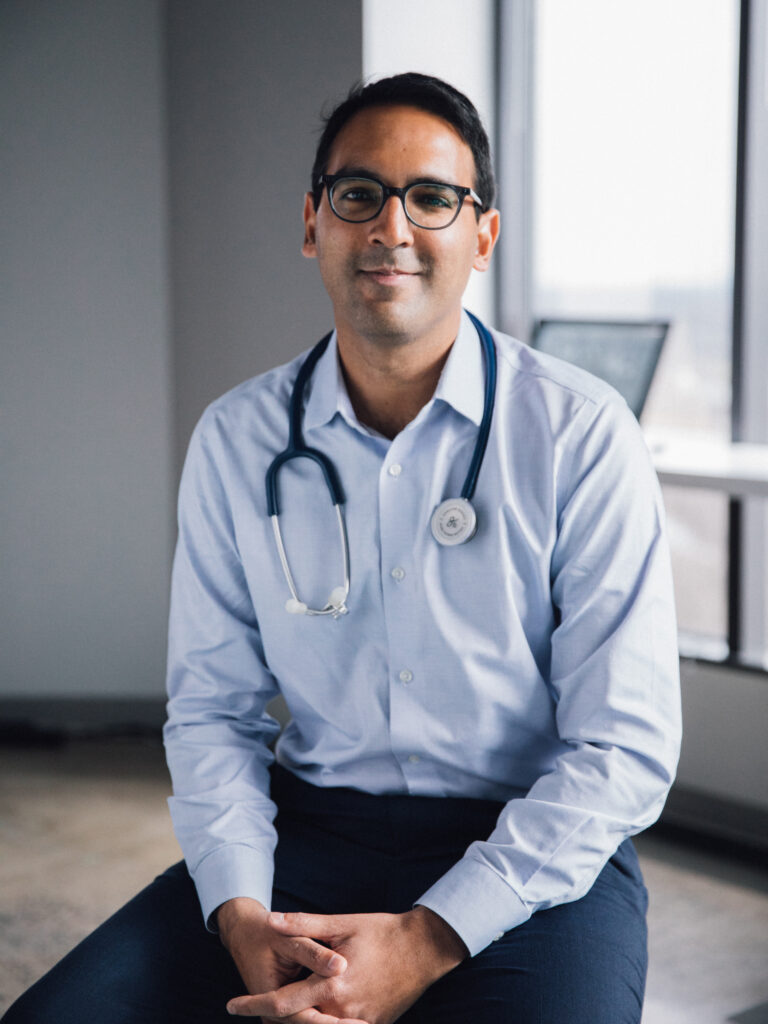
2006 Paul & Daisy Soros Fellow Shantanu Nundy’s career brings together so many essential (and usually disconnected) ingredients in health systems innovation. He studied engineering at MIT where he first encountered underserved populations through working in India teaching English. In studying medicine at Johns Hopkins, he developed checklists for the ICU and worked issues around patient safety. After business school at the University of Chicago, Shantanu began applying his interdisciplinary background while still in residency by launching SMS-DMCare, an automated text messaging software for individuals with diabetes, one of the first mobile health interventions to be adopted by the World Health Organization.
Since then, Shantanu has built new tech-enabled clinical models and population health programs at Evolent Health, led the growth of The Human Diagnosis Project, the world’s largest open medical project, to span 80 countries, and advised developing countries on digital health adoption as a senior health specialist at the World Bank. Now he serves as chief medical officer at Accolade, developing personalized navigation and population health services to companies that cover over two million working Americans. Throughout all of these roles pushing forward health systems innovation with technology, he’s maintained an active clinical practice as a safety net primary care physician in the Washington DC area.
Shantanu draws from each of these unique perspectives in casting a powerful vision for what our healthcare system could be. He makes the case in his new book Care After Covid: What the Pandemic Revealed Is Broken in Healthcare and How to Reinvent It that the future of healthcare is distributed, digitally-enabled, and decentralized–three fundamental shifts that form the basis of a framework for how healthcare can be redesigned in a post-pandemic world.
Shantanu opens each chapter with a poignant patient anecdote that illuminates a set of gaps and shortcomings of our current healthcare system. Each chapter includes a vision of where our healthcare system needs to go to fill those gaps, outlines what it would take to realize that vision, and ultimately offers a set of specific actions for each stakeholder in the healthcare system.
In reading through Care After Covid, I was captivated by the voice that Shantanu gives each of his patients, each of whom have been failed by the system in some manner. Just as the specific shortcomings become clear, Shantanu brings a refreshing sense of clarity and an achievable blueprint for how our system could be changed for the better. Each insight is practical, yet thoughtfully woven from his clinical experiences, business acumen, engineering mindset, and a palpable passion for the underserved. I found Care After COVID essential reading for any aspiring physician innovator and anyone in healthcare working towards our post-pandemic “new normal.”
I spoke with Shantanu in April of 2021 about his new book.
There are so many places we could dive in, but I wanted to ask if you could first give an overview of the origin behind this book. What inspired you to write Care After Covid?
In the first month of the pandemic, everyone was obsessed with testing–How can I get tested? Where is testing available? As someone who is wired to figure out simple solutions to things, I began asking the question, “Why can’t patients test themselves?” I was chatting with a friend, and she said why don’t you write this up? And so, we wrote this piece and it was the closest thing to a nerdy publication that went viral.
It was insane, I was getting calls from Senator Chuck Schumer’s office, featured in Rolling Stone magazine, USA Today, etc… It was really interesting because for the first time in my life I was starting to talk with policymakers, FDA, Congress, and people were saying really surprising things to me: How do we trust patients to do this right? Won’t they overuse it? How can we get results to patients? And that was when I realized some of these folks were disconnected from reality, and that I could take some of my experiences to be part of a national conversation. So that really was the origin, you’re seeing the country fall apart and I have an idea for how we can make a couple parts of this better, and I wanted to start by putting my own ideas down.
You broke down your book into ten thought-provoking chapters that each fall into three fundamental shifts enabling the future of healthcare. Without asking you to give too much of your book away, can you share each of these shifts behind your framework and a quick overview of what it means?
One of my mentors once told me, “words create worlds,” and I think part of the book was to deliberately create a new set of words to describe where we need to go. It was important to come up with concepts that shifted minds. Because healthcare is full of amazing creative people, helping each of us think differently is a higher leverage point than prescribing specific solutions. So, these three ideas were set up as counterpoints to common terms used by the healthcare industry that I believe are falling short of the vision I think we need:
- “Distributed” is a counterpoint to just virtual care or home-based care. It’s the idea that care should more often happen where patients are, which is at home, in the community and often on their mobile phones. But it recognizes that ultimately many patients will need to be seen in a clinic or hospital and that the whole experience needs to be integrated and seamless.
- “Digitally-enabled” is a counterpoint to the traditional AI or digitization of healthcare. By saying “digitally-enabled care” you’re actually taking care between two people and you’re using data and technology to strengthen that relationship. So you’re fundamentally changing that care model as opposed to digitizing it or trying to replace it.
- “Decentralization” is a counterpoint to value-based care. To me that’s only half the solution. Rather than just having providers be financially responsible for patients, you actually have to give them power– you have to allow them to change their care model and know who’s at risk. The same goes for patients, rather than “here’s an app or website for you,” you have to give them actual resources to make more of their own care decisions.
One of the topics I found relevant as I begin to enter my own third-year rotations in medical school is how we can make healthcare more patient-directed. You share a few examples of why information alone may not be enough or sometimes even too overwhelming for our patients. Can you share how we can best empower our patients in a more patient-directed world?
Having been in digital health for a little while now, the first wave of companies was really an information phase: like what Google did for the Internet. The amazing transformation that has happened in digital health with this new wave is that we’ve realized that information is necessary but not sufficient. So now what we’re seeing in this next wave is full-stack healthcare services that aren’t just a layer in the healthcare system, but companies that are delivering a full stack service including doctors and other healthcare professionals, processes and technology.
In a patient-directed world, we have an opportunity to redesign the care model—to think about who is the population, what’s the outcome we’re trying to get to, and how can we work backward to understand how to design the system. How can we create a core experience that just works? Rather than giving users a complicated setup manual, laptops today come 25 percent charged with a button that just turns on the computer and guides the user through the entire onboarding process. There’s this fallacy where we say, “let’s just help our patients figure out our broken system”, rather than saying “let’s make the system less broken.”
One of the issues you’ve thoughtfully weaved throughout your book is how COVID-19 has magnified the disparities in our healthcare system for racial and ethnic minorities. Can you share more on this and what gaps you’d encourage the medical field to focus on to avoid these systematic disparities?
I’m pretty concerned by the current discourse around the solutions. On one end, I feel like there are those who are working on pure advocacy that sometimes has too grand of a “pie in the sky” view. But on the other end, I’m worried about solutions that are very narrowly focused on these specific populations.
My argument is to start small and build for scale; to focus on the core of the experience. If you map out and design the experience for those who need it the most that will scale for many more people.
For example, take Accolade—what our founders realized is that the secret front door to healthcare was the number on the back of your insurance card. Rather than answering that with a robot or an IVR menu, a human being who knows you and your data picks up the phone. We didn’t say we’re only going to pick up the phone only for certain patients. We said we’re going to have someone pick up the phone for anyone who has a question or health need.
The result is that if you look at the people who call that number, it’s the people who are most in need. We have higher usage of our service by traditionally underserved populations. It wasn’t because we were specifically going after that population. It’s because we built a service that was solving a real problem—a problem that is shared by everyone but most especially by people who need it most.
We have this moment right now with health equity, where Fortune 100 companies and the CDC are putting equity front in center. But I worry that if we don’t offer real solutions we may waste this opportunity.
One of the most memorable sections and calls to action in your book is this realization that “our patients are waiting for us.” I wanted to ask if you could share more about this palpable sense of urgency that I felt as I was finishing your book and why we are at an important inflection point.
Pandemics like Covid-19 only happen once in a century and we have a narrow window to move the healthcare system forward. When you have broad recognition and discussions happening from your neighborhood to corporate America to the halls of policymakers, you have a moment. We’ve already demonstrated that healthcare can change and that patients are ready to embrace that change.
Look back to how an under-resourced clinic like mine went to 80 percent virtual in just a couple of weeks. More broadly, we’ve trained by experience a generation of nurses and doctors in public health: looking at data, proactively reaching out to patients, and implementing novel solutions.
What we need to do next now is seize this moment to create the healthcare system our patients have been waiting for.
What do you hope readers will take away most from your book?
The biggest takeaway is being really clear on what the vision for healthcare is—what does “good” look like? Right now, as we’re talking, there are hospital executives saying, “virtual is bad for business: marginalized patients had bad access to it, providers had trouble logging in. Should we go back to all in-person?” There are policymakers asking, “we relaxed patient privacy policies for a few months, but should we just flip that back on?”
These conversations are happening because we’re not really clear on what “good” is when it comes to healthcare. If you’re clear on that then that becomes what you’re solving for. So, it’s not “should we go virtual?” it’s, “we’re going virtual and becoming distributed. How can we do it in a way that is inclusive, that is comprehensive and not transactional, and driven towards outcomes?” We’re still in a place where we’re debating the end goal and that’s slowing us down.
Look what the Biden Administration accomplished by putting a Big Hairy Audacious Goal (BHAG) of trying to vaccinate x many people by y date. The usual way we try to change healthcare is to train physicians on administering the vaccine, create a code to bill for the vaccine, form patient advocacy groups, etc. But that wouldn’t have worked.
Outside of vaccine rollout, we don’t talk enough about actual goals—we need to put some real markers out there. What would some goals look like? “20 percent of hospitalizations in five years will be at home,” or “90 percent of hypertensive patients well-controlled on medications”. These goals orient the entire machine in an “all-in” systems approach to get to something that matters to real people and can move our system meaningfully forward.
Rewinding back to your days in medical school, how did the PD Soros Fellowship influence your career trajectory?
For me, receiving the Paul & Daisy Soros Fellowship for medical school was transformative. It was the first time an organization really came to understand me as a person and said, “We believe in you.” That has emboldened me to swing harder in my career and to more openly be my best self. I’m so grateful for that.
2020 Paul & Daisy Soros Fellow Sherman Leung is studying medicine at the Icahn School of Medicine at Mount Sinai. He invests in and launches healthcare companies at AlleyCorp, a venture studio and early-stage investment fund based in New York City. Sherman cares deeply about leveraging technology to support underserved patient populations and increasing the efficiency and efficacy of health care delivery. You can sign up for his newsletter, Margins of Medicine, on systemic disparities in healthcare here. ∎
Featured Fellows
-

Shantanu Nundy
Chief Medical Officer, Accolade
Shantanu Nundy is an immigrant from Canada. Fellowship awarded in 2006 to support work towards an MD in Medicine at Johns Hopkins University
-

Sherman Leung
Emergency Medicine Resident, Stanford Healthcare
Sherman Leung is the child of immigrants from Hong Kong. Fellowship awarded in 2020 to support work towards an MD in Medicine at Icahn School of Medicine at Mount Sinai
Keep Exploring
-
 Read more: NOT ON MY RESUME: Jamaji C. Nwanaji-Enwerem
Read more: NOT ON MY RESUME: Jamaji C. Nwanaji-Enwerem- Fellow Highlights
- Fellows in Action
NOT ON MY RESUME: Jamaji C. Nwanaji-Enwerem
-
 Read more: New Play by 1999 Fellow and Former Ambassador Julissa Reynoso Opens at The Public Theater
Read more: New Play by 1999 Fellow and Former Ambassador Julissa Reynoso Opens at The Public Theater- Fellow Highlights
New Play by 1999 Fellow and Former Ambassador Julissa Reynoso Opens at The Public Theater
-
 Read more: The Public Voices Fellowship of PD Soros, in partnership with the Oped Project: Year Four
Read more: The Public Voices Fellowship of PD Soros, in partnership with the Oped Project: Year FourThe Public Voices Fellowship of PD Soros, in partnership with the Oped Project: Year Four
-
 Read more: NOT ON MY RESUME: Ming Hsu Chen
Read more: NOT ON MY RESUME: Ming Hsu Chen- Fellow Highlights
- Fellows in Action
NOT ON MY RESUME: Ming Hsu Chen