- Fellow Highlights
Sunita Puri: In the Borderlands Between Life & Death
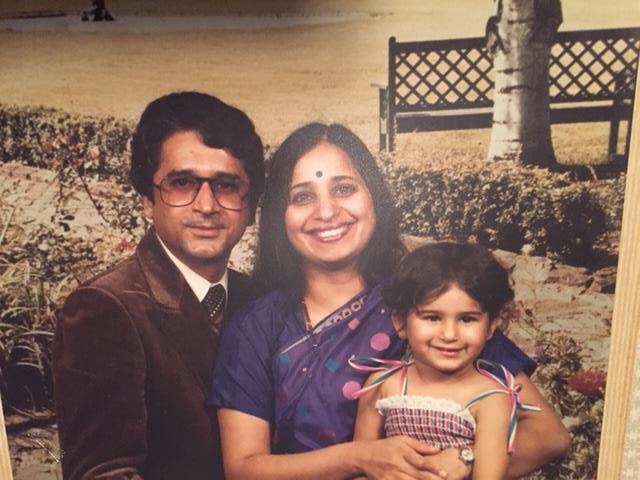

Looking out over a Kentucky sunset one evening when 2004 Paul & Daisy Soros Fellow Sunita Puri was five, her father and her marveled at the beauty of the disappearing sun. In describing the sight before them, Sunita’s father told her about impermanence; the day’s impermanence, and peoples’ impermanence, too. That was the first time that Sunita considered death—a topic that has become the center of her professional life as a palliative care doctor, and which is at the heart of her memoir, That Good Night: Life and Medicine in the Eleventh Hour.
Sunita, who is the medical director of the Palliative Medicine and Supportive Care Service at the Keck Hospital and Norris Cancer Center of the University of Southern California, writes about what she has learned while working “in the borderlands between life and death.” That ongoing proximity to death has transformed the way that Sunita practices medicine, but it has also given her a wealth of experience that will help readers understand what they might want when they find themselves in the positions of Sunita’s patients.
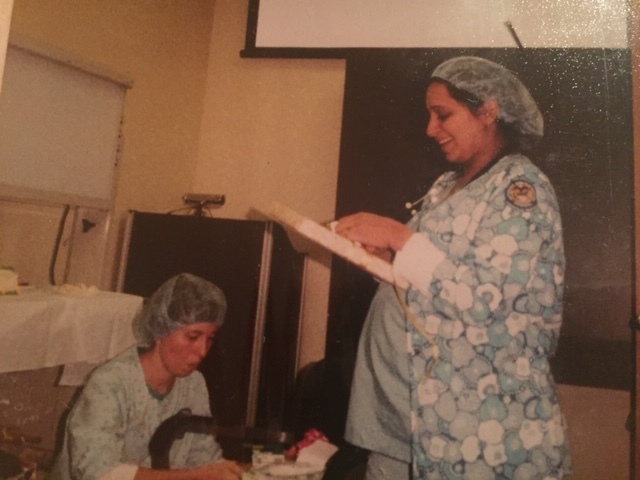
Much of Sunita’s own training as a doctor focused on the absolute rejection of death; the mantra was to defend the patient against death at all costs, no matter how close to death the patient might be, or how much additional pain might be caused.
“I began to believe that a longer life was a better life. A doctor’s job was to manipulate, control, and postpone death, not to accept it as inevitable. We learned to rage against the dying of the light,” Sunita writes.
That attitude about death is also one that her patients and their families often express. Families and patients might demand that their doctors “do everything” to keep the alive. But what does “do everything” mean? Sunita unravels this question again and again within the varied circumstances of her patients’ cases; each time revealing a new element of the demand.
Documenting the intimate inflection points of her time with individual patients, Sunita shares a vulnerability and sense of humility in her book that is uncharacteristic of doctors in today’s world—she shares her sense of relief when a patient ends a conversation before asking what Sunita anticipated to be questions she couldn’t answer; the realization that she had endangered a patient when she made a home visit in her scrubs, making it clear a doctor had likely dropped off expensive prescription medicines; the feeling of her anger overcoming her empathy as she talked with a livid family member about their loved one’s care; and her thoughts as a patient’s loved one sobbed and convulsed as he begged Sunita to make sure his wife felt no pain in her final minutes of life.
The Power of Communication
Sunita believes in the power of communication—she must be able to talk to her patients and their families about death. What are their expectations? What are their fears? What are their hopes and wishes? Without a clear understanding of the answers to these questions, it can be difficult to know what the best palliative care options are for them.
Harder than asking those questions, is how those questions are asked. “How you walk into a patient’s room and tell them you’re from the palliative care team—how you explain that, and whether you do that well, can be the difference between whether a patient and their family are open to you and to the crucial care you can provide or not,” Sunita explained in an interview ahead of the launch of the book.
“You are forced to a place of extreme intimacy, talking to them about the lives they have led up to this point, their fears and regrets, the people they love, the ways they have made sense of loss earlier in their lives, and how they are making sense of loss now, in the days or weeks or months they may have left to live,” Sunita writes.
“You must act as if it is normal for a doctor to ask these probing questions during the first or second meeting with them. Because if you act awkward, they will wonder why you are here.”
“Many people who have these conversations know that they are important, but in the absence of training they can be challenging,” Sunita explained.
Sunita looks for the “pivotal moments” that allow her to help families align their hopes and expectations with the medical care that is possible. For a patient in the intensive care unit whose organs are failing because of irreversible causes and whose family would like every manner of support, Sunita says it can be challenging to pause and ask questions.
“An earlier version of myself might have thought, ‘Okay, a patient and their family want this; I have to keep it going.’” Now, faced with that situation, she sees an opportunity to ask a family about what they are hoping for—and if a family is hoping for, say, their loved one to recover and come home—that’s often a good opportunity for Sunita to help the family better understand the patient’s situation.
Raised on Faith
Salvation. Miracle. God’s plan. Heaven. Prayer. While these are not traditionally thought of as medical terms, they are ideas that are fundamental to end of life care.
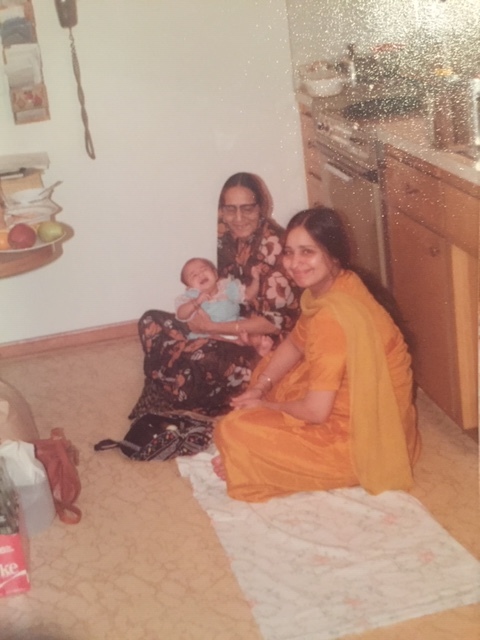
Sunita’s first education in faith came from her parents, who both grew up in poverty in India. “The thing that propelled them to the lives they have now is having this scary deep faith in God and the workings of the universe,” Sunita explained. “They attribute everything that has happened to them, good and bad, to something that God has given them to learn from.”
Some of Sunita’s first words were prayers. As a child, she prayed for hours each week, recited mantras, and would follow her father around the house each night as has he acknowledged every picture of God.
Years later, when Sunita was in medical school, and her father had to undergo surgery, Sunita’s mother, who is also a doctor, asked the surgeon to tape a photo of the Hindu deity Lord Ganesha to his chest. “I know you will take good care of him, but I need God to take care of him, too,” her mother told the surgeon who was happy to oblige her request.
Sunita’s mother’s attention to faith was not unlike some of Sunita’s own patients. But while Sunita may have understood religion in her personal life, she had to learn how to talk about it within the context of her work. One mentor, Christina Nguyen, was instrumental in this regard. She taught Sunita the power of a deep breath before speaking, which allowed her to draw on “strong emotions—both hers and others’—to disperse before making her point.”
Most importantly, she taught Sunita how to ask about her patients’ and their families’ faiths, and how to connect with them in a language of faith. Talking with a couple who had a dying son, Dr. Nguyen told them that they would know God was calling when their child’s heart stopped. “God’s call. A tiny phrase I had never heard in a medical conversation. Two words that said something enormous, eternal: dying is spiritual, not just medical. The moment of death can be sacred,” Sunita wrote of the conversation.
Regardless of faith, the idea that death can be sacred, is Sunita’s gift to her readers. Each chapter’s encounter with death is a reminder to live deeply—and to find it in ourselves to prepare for our own good night. ∎

Read more: “The Lesson of Impermanence” by Sunita Puri in The New York Times.
Watch: “Physician & Author Sunita Puri on End of Life Care” featuring Sunita Puri on PBS.
Keep Exploring
-
 Read more: Q&A with MD/PhD Student Silvia Huerta Lopez
Read more: Q&A with MD/PhD Student Silvia Huerta LopezQ&A with MD/PhD Student Silvia Huerta Lopez
-
 Read more: PD Soros Eligibility Guide for PhD Applicants
Read more: PD Soros Eligibility Guide for PhD Applicants- Applicant Information
PD Soros Eligibility Guide for PhD Applicants
-
 Read more: Watch: Optional Exhibits & Recommendations
Read more: Watch: Optional Exhibits & Recommendations- 2025 Information Sessions
Watch: Optional Exhibits & Recommendations
-
 Read more: Watch: Essay Writing information session
Read more: Watch: Essay Writing information session- 2025 Information Sessions
Watch: Essay Writing information session
